Speaker: Dr. Stephen Williams, United States
Important Takeaways
-
Dr. Stephen Williams discussed updates to AUA and EAU guidelines, focusing on stratifying non-muscle-invasive bladder cancer (NMIBC) by risk.
-
Urine biomarkers should not replace cystoscopy for diagnosis and surveillance, given the lack of robust evidence.
-
Treatment options have evolved to include newer chemotherapy regimens like Gemcitabine and BCG alternatives for relapsed cases.
-
EAU guidelines introduce "very high-risk" stratification and emphasise radical cystectomy for non-responders.
-
Intermediate risk classification aims to differentiate between favourable and unfavourable cases, simplifying treatment decisions.
Key Highlights
Guideline Overview and Risk Stratification:
Dr. Williams began by reviewing the evolution of NMIBC guidelines from AUA (2016) and EAU, both of which categorise bladder cancer patients into low, intermediate, and high-risk groups. EAU guidelines take it a step further with a “very high-risk” classification, targeting aggressive management early on.
Urine Biomarkers and Cystoscopy Use:
While urine biomarkers are discussed in the guidelines, clinicians are advised not to replace cystoscopy with them, particularly for patients with low-risk NMIBC. There is currently insufficient evidence to justify routine biomarker use for follow-ups.
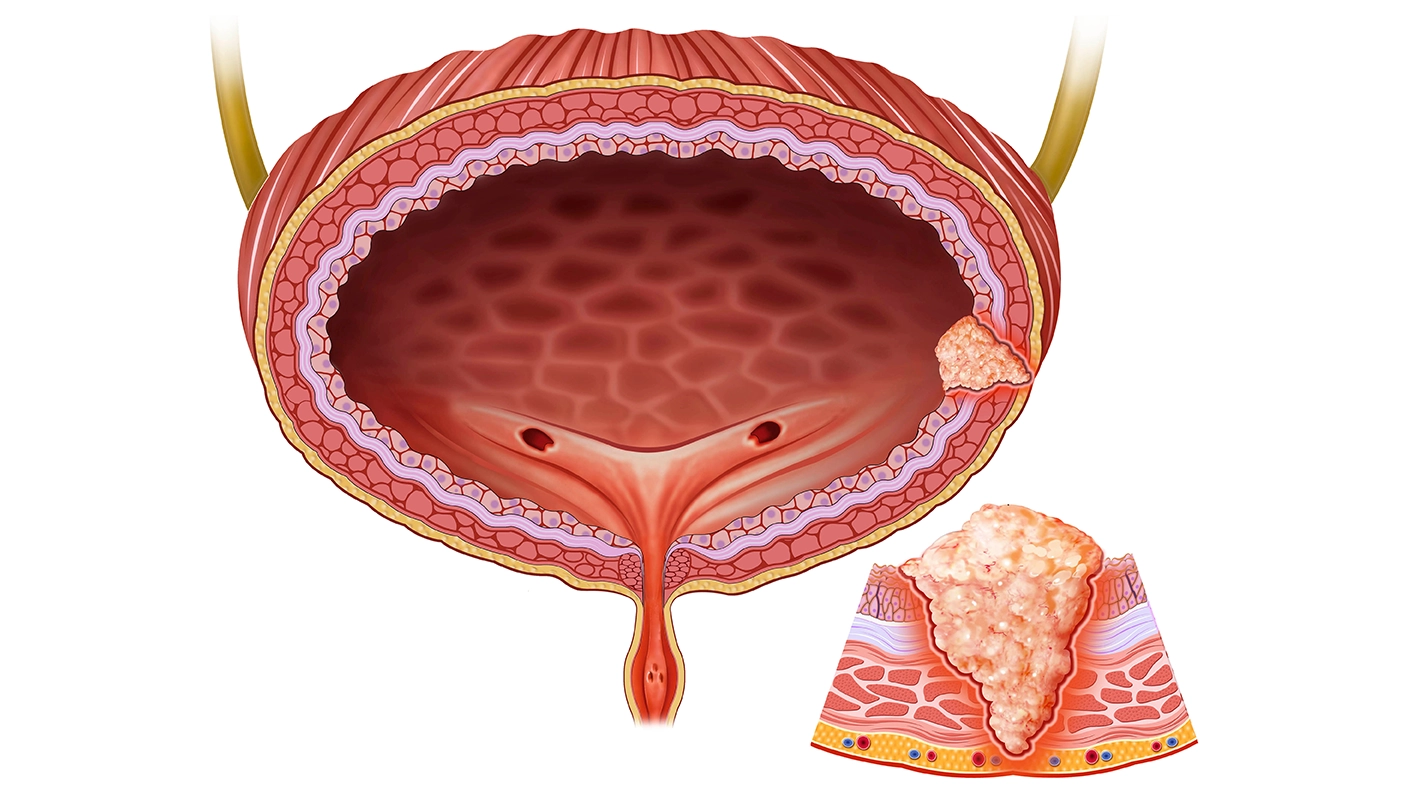
Intravesical Therapy and Evolving Chemotherapy Regimens:
Treatment modalities for intravesical therapy have shifted from traditional mitomycin to newer agents such as Gemcitabine. BCG remains a cornerstone for relapse management, with additional therapies like pembrolizumab emerging as salvage options.
Intermediate and Very High-Risk Classification:
The EAU’s approach includes further stratification within intermediate-risk patients to identify unfavourable cases requiring more aggressive interventions. Radical cystectomy is recommended for patients not responding to intravesical therapy, especially those classified under "very high-risk."
Simplifying Treatment Protocols:
A major challenge, according to Dr. Williams, is balancing complexity with clarity in intermediate-risk categorization. The goal is to streamline treatment paths while avoiding unnecessary complications caused by overlapping risk criteria.
Pathologic Review and Diagnostic Challenges:
Dr. Williams highlighted the importance of re-evaluating pathology when there are doubts, especially for TA high-grade cases. Muscle presence in specimens remains a key factor, and AI tools are being explored to assist in treatment decision-making.
The Role of Simplifying Risk Stratification
There is a call for streamlined approaches in NMIBC management to reduce complexity for general urologists, aiming to make guidelines more accessible without compromising patient-specific risk assessment accuracy. The IBCG model was acknowledged as a valuable tool, though complex, to identify patients needing escalated intervention.
Panel Discussion Highlights:
-
Question on TA High-Grade Tumours: Many practitioners favour treating high-grade TA lesions as high-risk, similar to T1, given the ambiguity in predicting outcomes in the intermediate-risk group.
-
Pathology Reviews: For high-grade lesions with questionable pathology, panellists agreed on the importance of second opinions or centralised pathology reviews.
-
AI and Digital Pathology: Emerging AI-based pathology tools (e.g., Valar Labs) are becoming instrumental in categorising patients’ risk profiles, especially those on the cusp of high-risk classifications.
Dr. Williams concluded by emphasising that while guidelines serve as essential frameworks, personalised assessment remains key, especially as new therapies and digital tools continue to evolve in NMIBC management. The session’s consensus was that simplifying the complex guideline structure could enhance guideline adherence and improve patient outcomes in routine urology practices.
Société Internationale d'Urologie Congress, 23-26 October 2024, New Delhi, India.