EAU 2024: Case Discussion: Surgical Treatment for Detrusor Sphincter Dyssynergia (DSD) is the way to go by Dr B. Blok
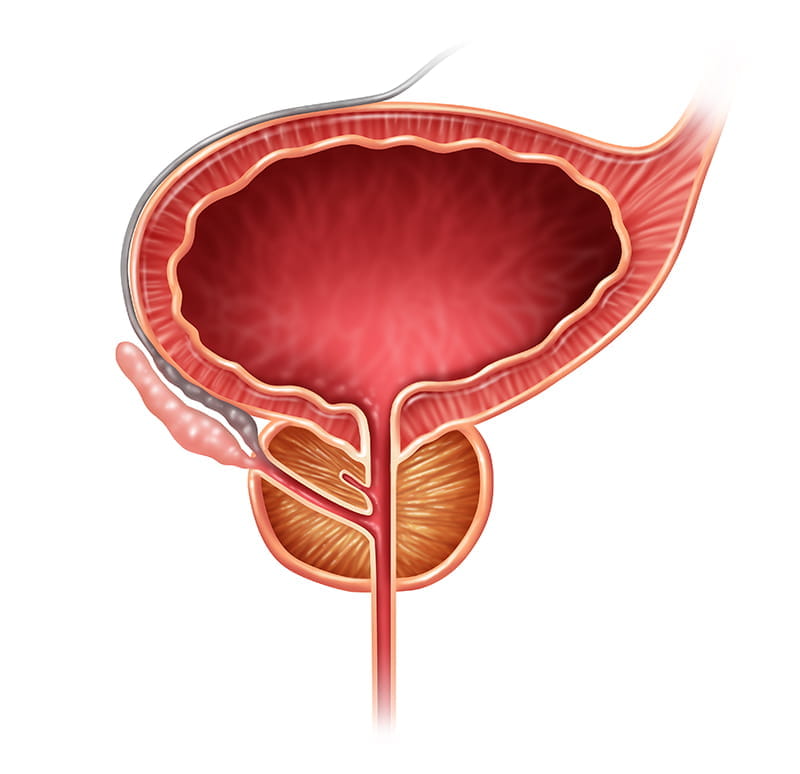
The moderator, Dr B. Blok, presents a case of a 53-year-old male who sustained a complete spinal cord injury at the C5 level three years ago. Initially advised to undergo clean intermittent catheterization (CIC) four to five times daily along with oxybutynin twice daily by the spinal centre, the patient declined due to concerns about loss of independence. Currently, he relies on reflex micturition utilizing a condom catheter administered once daily by a caregiver in the morning, with an average volume of 300 mL. Abdominal ultrasound revealed a distended bladder without hydronephrosis or diverticula; kidney function remains normal. There have been no episodes of autonomic dysreflexia or fever. Genomic investigation indicates detrusor overactivity and detrusor sphincter dyssynergia, characterized by rapidly increasing detrusor pressure to 60 cm H2O at 200 mL during the filling phase, persisting until cessation of filling. During micturition attempts, detrusor sphincter dyssynergia is observed, with a post-void residue of 350 mL.
(Yes) Surgical Treatment for Detrusor Sphincter Dyssynergia (DSD) is the way to go by S. Musco
The argument is for surgical treatment in quadriplegic patients, particularly in cases of detrusor sphincter dyssynergia (DSD) associated with high blood pressure and post-voiding residuals. Long-term complications, including stones, hydronephrosis, vesicoureteral reflux, and symptomatic febrile urinary tract infections (UTIs), are highlighted as significant concerns. The focus is on the unique challenges faced by quadriplegic individuals, particularly those with limited independence in daily activities and greater reliance on caregivers. Intermittent catheterization, often difficult to manage in quadriplegic patients due to caregiver availability and economic constraints, is presented as less favourable compared to surgical intervention. Alternative treatments like alpha-blockers and botulinum toxin A injections are deemed inadequate due to limited efficacy and short-term data. Long-term reliance on indwelling catheters is discouraged due to associated complications. Ultimately, surgery is proposed as the most definitive solution to improve the quality of life for quadriplegic patients with DSD.
Sphincterotomy has been a longstanding approach, with the initial procedure performed approximately 60 years ago by Gross. However, contemporary understanding suggests that the "mother's bucket" method is the preferred and safer technique. This method involves an incision at the intermediate position, around 12 o'clock, as it carries a lower risk of bleeding and erectile dysfunction. Additionally, advancements allow for the use of laser techniques in performing sphincterotomy, with favourable functional outcomes. Sphincterotomy effectively addresses post-voiding residual issues, especially in patients with levels exceeding the normal threshold of 200 millilitres, resolving concerns in approximately 70 to 90 per cent of cases. Even for patients with persistently high post-voiding residuals, such as our case with levels exceeding 350 millilitres during the urodynamic assessment, the benefits outweigh the associated risks of sphincterotomy, which include minimal risk of bleeding and erectile dysfunction, affecting less than 10 per cent of cases. Although sphincterotomy may require repeat procedures over time, its benefits are long-lasting, often extending beyond 10 years, making it an effective and clinically sound intervention aerodynamically and clinically.
In conclusion, there is currently no effective conservative treatment for DSD. Sphincterotomy remains the primary treatment for this condition. It is the first choice for patients unable to perform intermittent catheterization to ensure independence in their recovery. Sphincterotomy has also shown efficacy in patients with high-risk factors such as high blood pressure. Despite the possibility of complications, as observed in the case, it is important to note that sphincterotomy can be safe and effective even in very high-risk patients with upper urinary tract damage.
(No) Surgical Treatment for Detrusor Sphincter Dyssynergia (DSD) is the Way to Go by Barbara Padilla-Fernandez
The speaker, Barbara Padilla-Fernandez, acknowledged that sphincterotomy had emerged as a promising alternative for the patient, but she questioned whether the patient’s decision was truly optimal at that time. Three crucial points were considered: Firstly, why did the patient refuse catheterization, often considered the best option? Additionally, alternative non-invasive options to sphincterotomy were explored, referencing pertinent studies.
Understanding patients' reluctance toward intermittent catheterization was vital. Studies indicated common concerns such as fear of the unknown, uncertainty about procedure execution, and doubts regarding its impact on quality of life. There was also the fear of pain and shame associated with spinal cord injury-induced incontinence. Patients who had attempted catheterization may have cited inconvenience, frequent infections, or reluctance to depend on others.
Addressing these concerns was pivotal. Prophylactic measures could mitigate infection risks, while discussions about catheterization techniques and caregiver support may have alleviated inconveniences. Recommending a wider catheter for faster bladder emptying could also have been beneficial. Moreover, recognizing the emotional toll of spinal cord injury and offering support for depression was essential.
A comprehensive review of the patient's catheterization technique, assessment of caregiver support adequacy, consideration of prophylactic measures, and potentially exploring alternative catheter options were warranted. By addressing these factors, the patient's comfort could have been enhanced, complications minimized, and overall quality of life improved.
In discussing urinary catheterization techniques, it was evident that women faced particular challenges, especially with lesions lower than the presented case. Studies indicated that performing catheterizations multiple times a day consumed a considerable portion of their time. Additionally, issues with restroom accessibility and hygiene posed further obstacles, especially when away from home. These barriers underscored the complexities involved.
Moving on to sphincterotomy, while it presented a viable option, patients had to be informed about potential side effects such as haemorrhage, erectile dysfunction, retrograde ejaculation, and the risk of urethral stricture or fistula formation. Chronic incontinence was also a concern with condom catheter use, along with the possibility of ulcers. Considering non-invasive alternatives, botulinum toxin injections had shown promise in improving void and detrusive pressures, flow rate, and post-void residual urine. However, while some patients experienced enhanced micturition quality, others faced increased incontinence, leading to dissatisfaction.
The speaker centred around the treatment of neurogenic patients with toxins, particularly focusing on detrusor injections ranging from 200 to 300 units, which have shown significant therapeutic effects. Additionally, injections into the urethral sphincter were mentioned as an alternative for treating detrusor sphincter dyssynergia, albeit with potential side effects such as urinary incontinence and frequency. This method serves as a temporary solution, providing an alternative to surgical sphincterotomy. Dr. Blok's suggestion of using urethral stents, both temporary and permanent, was also highlighted, although the latter was noted to carry a high complication rate. Addressing concerns about catheterization in patients, prophylactic treatment for potential urinary tract infections was recommended, along with ensuring patients are informed about the side effects of sphincterotomy. Non-invasive treatments were discussed as well, acknowledging the need for repeated procedures despite their benefits.
Discussion
An inquiry raised revolved around potential disparities in the efficacy of botulinum toxin treatment between male and female patients with spinal cord injury. The discussion suggested that while women may exhibit better outcomes with botulinum toxin, particularly concerning the sphincter, this advantage does not extend uniformly to all areas, such as the bladder. Concerns arise regarding the management of urinary incontinence in women, which may be more complex due to factors like sphincterotomy and the use of PETs rather than condoms. The management of incontinence in men, on the other hand, may be facilitated by the use of a Uro-condom catheter. Additionally, the risk of bed sores in paraplegic patients poses a limitation to treatments aimed at increasing incontinence, prompting a cautious approach. Overall, the discussion highlights the nuanced considerations involved in administering botulinum toxin treatment to patients with spinal cord injury, particularly in managing urinary incontinence in both men and women.
A pertinent question was raised regarding the viability of convincing patients to undergo irreversible surgery, particularly when better solutions may emerge in the near future. While acknowledging the patient's concerns, it's noted that despite over 60 years of questioning, no alternatives as effective as sphincterotomy currently exist. However, there is recognition of the need to explore non-destructive alternatives. Suggestions include the possibility of more effective neuromodulation systems in the future, particularly for patients with complete spinal cord injuries. While acknowledging potential solutions for different types of patients, such as those with multiple sclerosis versus complete quadriplegia, it's emphasized that sphincterotomy doesn't preclude future options like artificial sphincters for continence. Botulinum toxin A is proposed as an interim measure to assess the patient's response before committing to surgical intervention. Moreover, the mention of a recent grant for bilateral pudendal nerve stimulation at 10,000 hertz offers hope for temporary sphincter blockage, particularly in neuro-urological patients, suggesting ongoing exploration of alternative treatments.
European Association of Urology (EAU) Annual Congress 2024, 5th April - 8th April 2024, Paris, France