Introduction
Ovarian hyperstimulation syndrome (OHSS) is a rare, iatrogenic complication of the luteal phase or/and early pregnancy after ovulation induction or of ovarian stimulation. Complications of OHSS include ascites, hemoconcentration, hypovolemia, and electrolyte imbalances.
The prevalence of infertility is increasing and so are the ovulation induction practices and use of assisted reproduction technology. Hence, it is important that the healthcare practitioners become familiar with the factors that predict risks of OHSS for its effective management.
Prediction of OHSS
|
Anti-Mullerian Hormone (AMH) |
A larger cohort of smaller antral follicle may be indicated by high AMH value and a higher risk of OHSS. |
|
Antral Follicle Count (AFC) |
2/3D transvaginal ultrasound used to count every follicle between 2-10 mm between days 2 and 4 of a spontaneous menstrual cycle in the absence of a follicle > 10 mm. |
|
Basal Follicle Stimulating Hormone (FSH)* |
Indirect marker of functional ovarian reserve. |
|
Inhibin - B* |
Higher inhibin B concentration during gonadotropin stimulation and on the day of oocyte retrieval in patients who later develop ovarian OHSS. |
|
Age* |
Young women are more likely to suffer from OHSS (<35 years). |
* Lower predictive accuracy
|
Serum estradiol levels |
Marker of increased granulosa cell activity. OHSS can be predicted by absolute high or rapidly rising values of estradiol. |
|
Medium/large follicle count |
The risk of OHSS increases with greater stimulation at the moment of hCG trigger. |
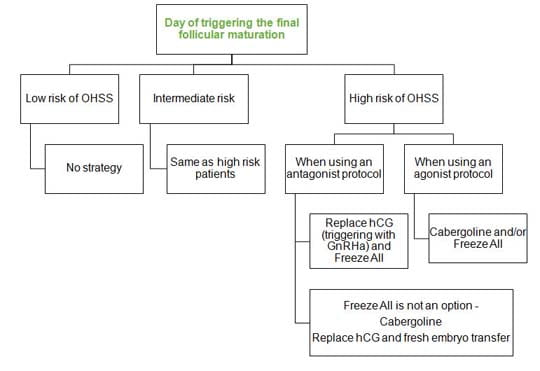
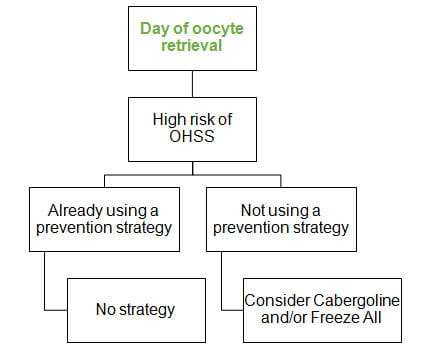
Strategies to Prevent OHSS
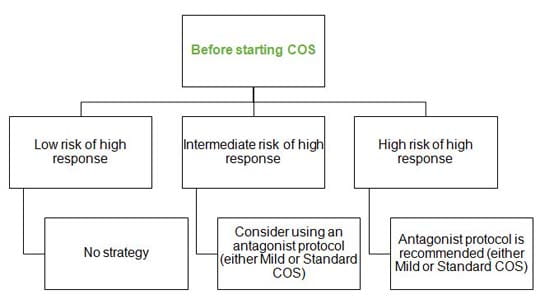
Low risk of high response - AMH ≤ 1 ng/mL and/or AFC ≤ 6
High risk of high response - AMH ≥ 3 ng/mL and/or AFC ≥ 16
Low risk of OHSS - ≤ 10 follicles ≥ 10 mm and/or estradiol < 1,500 pg/mL
High risk of OHSS - ≥ 18 follicles ≥ 10 mm and/or estradiol > 3,000 pg/mL
References
- Ultrasound Obstet Gynecol. 2014; doi: 10.1002/uog.14684
- J Assist Reprod Genet 2011;28(12):1197–1203
- Hum Reprod Update 2002;8(6):559-577