Introduction
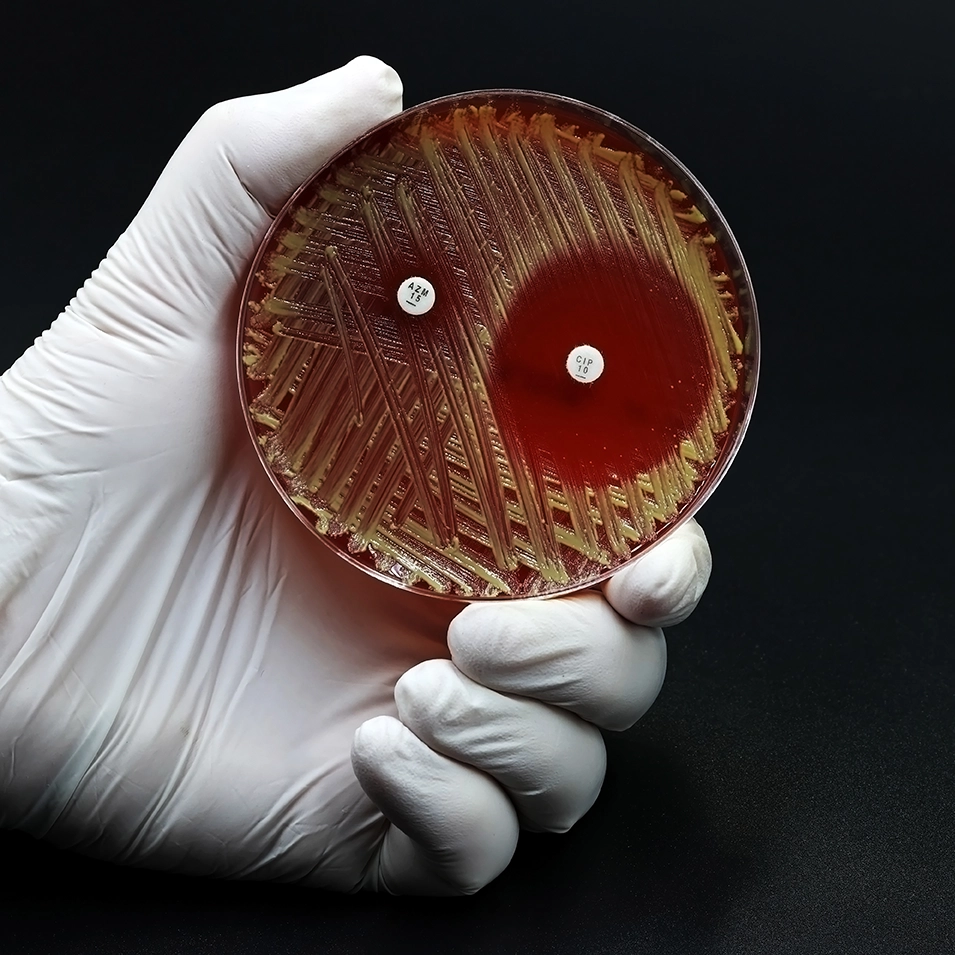
Methicillin-resistant (MRSA) is a recurrent therapeutic problem particularly in the intensive care unit and in the ventilated patients. It accounts for 10-40% hospital-acquired pneumonia. Vancomycin and linezolid both are currently recommended for the treatment of nosocomial pneumonia due to MRSA.
Aim
To compare a fixed linezolid dose to dose optimized vancomycin for the treatment of bacteriologically proven MRSA nosocomial pneumonia.
Patient Profile
- N=1225
- Patients with a bacteriologically documented MRSA infection
- Hospitalized adult patients presenting with MRSA pneumonia acquired in hospital or associated to care
Methods
- ZEPHyR Study (linezolid in the treatment of subjects with nosocomial pneumonia proven to be due to methicillin-resistant Staphylococcus aureus)
- Multicenter, prospective, double-blind study
Study Design
1225 patients were randomized to receive linezolid or vancomycin IV during 7 to 14 days.
Drug Dose
Linezolid IV: 600 mg every 12 hours
Vancomycin: Initial dose of 15 mg/kg IV every 12 hours, adjusted later according to the residual plasmatic rates.
Endpoint
- The main judgment criterion of the study was the rate of clinical success at the end of the study in the per protocol (PP) population
- The secondary judgment criteria were to rate microbiological eradication at the end of treatment and at the end of the study, the rate of clinical success at the end of treatment in the modified ITT analysis (mITT) and PP populations,
Results
Efficacy
- In the PP population, patients clinically cured at end of study
- 95 of 165 patients treated with linezolid (57.6%)
- 81 of the 174 patients treated by vancomycin (46.6%) (P = 0.042)
|
|
Linezolid group |
Vancomycin group
|
|
Success Rates (%) |
|
|
|
In patients with multi-bacterial infections |
55.6 |
43.1 |
|
In ventilated patients |
55.5 |
44.2 |
|
In cases of associated corticotherapy |
53.9 |
44.4 |
|
Survival Rates (%) |
|
|
|
the death rate at 60 days in the global ITT population (All causes) |
15.7 |
17.0 |
|
the death rate at 60 days (Pulmonary MRSA infection) |
28.1 |
26.3 |
|
Rate of Microbiological success (%) |
|
|
|
In PP population at end of study |
58.1 |
47.1 |
|
In PP population at end of treatment |
81.9 |
60.6 |
Safety
- The incidence of nephrotoxicity in the mITT population was
- 8.4% in the linezolid group
- 18.2% in the vancomycin group
- The incidence of renal toxicity, among patients treated with vancomycin, was higher when the residual rate of antibiotic at D3 was high:
- 37% for residual rates ≥ 20 µg/mL
- 22% between 15 and 20 µg/mL
- 18% below 15 µg/mL
Conclusion
- This study clearly suggested linezolid as a better alternative compared to vancomycin and should become the first choice treatment for nosocomial MRSA pneumonia.
- The superiority of linezolid was also reflected by the absence of renal toxicity.
Med Mal Infect. 2013; 43(11-12): 451-5. doi: 10.1016/j.medmal.2013.09.011.