The session discusses the concept of implementation science versus inventing new medications for heart failure with reduced ejection fraction. There are standard heart failure medications and devices that reduce mortality for patients with heart failure and a reduced ejection fraction. However, the benefit of new heart failure medical therapies compared to older ones has diminished returns with regards to reducing absolute 2y mortality rate and absolute 2y HF hospitalization rate. The medications such as Vericiguat and Omecamtiv have shown benefits when added to other therapies but meagre benefits in cardiovascular mortality. Instead of investing in developing new drugs, it is essential to focus on implementing the existing therapies for more patients, as many of the newer medications do not get approved by the FDA or are not priced appropriately. New medications have relatively small benefits on quantity and quality of life, On the other hand, the results from the PROMPT HF trial & STRONG HF trial have demonstrated that effective implementation and rapid titration of GDMT has better absolute mortality risk reduction. Hence it is imperative to focus on the proper implementation of existing GDMT for greater benefit in quantity and quality of life rather than investing heavily in the development of newer medicines that have lower absolute mortality benefits.
Progress has been made in heart failure treatment since 1987, including the discovery and implementation of ACE inhibitors, beta-blockers, and ICDs. If progress had been halted at any point, the benefits of subsequent treatments, such as SGLT2 inhibitors, would have been missed. So there is a need to keep progressing and discovering new pathways, as there is still a significant residual risk of heart failure even with current treatments. Genetics and precision medicine also play an essential role in treating heart failure to continue making progress every day.
Biomarkers are defined as objective characteristics measured and evaluated as indicators of biological processes, pathogenic processes, or pharmacological responses. In the heart failure area, the most commonly used biomarkers are NPs, TIC peptides, and genetic biomarkers. However, the clinical usefulness of biomarkers in heart failure is debatable, with low yield ratios for clinical usefulness. The American guidelines recommend the use of NPs, BNP, or anti-BNP for diagnosis and risk stratification. In contrast, the European guidelines are more conservative, suggesting only NPs in the diagnostic flow. Biomarkers are recommended as a reasonable diagnostic test for ruling out heart failure as a cause of breathlessness in specific settings. The evidence for biomarkers in acute or chronic heart failure is limited, and there is no gender specificity tested in various ethnicities. NPs are moderately increased in HFpEF. The levels fall to normal during symptom-free periods. The yield ratio and diagnostic value of biomarkers in heart failure are quite limited, particularly in stage D. However, biomarkers can provide some incremental prognostic value over standard approaches for cardiovascular risk assessment.
The trajectory of biomarkers is important for reverse remodeling, NP concentration, and lab ventricle reaction fraction is associated with cardiac modeling well before symptom changes. Biomarkers are widely used as surrogates for endpoints in clinical trials. Proteomics and a multi-marker approach are important for providing additional information for decision-making in conjunction with clinical data. In the future, biomarker-guided management of heart failure could potentially prevent adverse events.
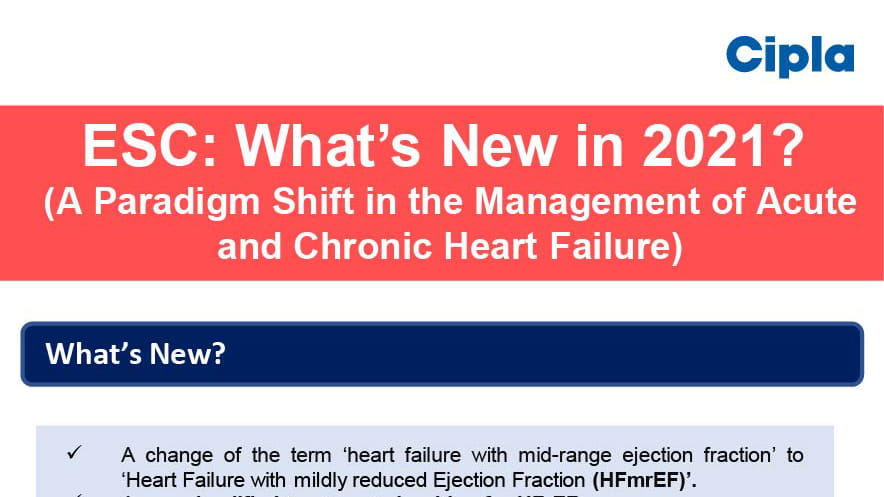
The distinct clinical entity of heart failure with mildly reduced ejection fraction differs from heart failure with reduced ejection fraction or HFpEF. Heart failure is a syndrome, not a diagnosis, and the guidelines help define its different components by breaking it down into stratification by ejection fraction. Patients with mildly reduced ejection fraction do better overall than those with reduced ejection fraction or HFpEF, but patients in this category are predominated by being in transition, with ejection fractions that are most likely to get better or worse. This category also offers clues to mechanisms underlying heart failure, and physicians should be precise with their approach to diagnosis, considering traditional hypertensive heart disease, myocardial infarction, fibrosis, and mimickers such as amyloid or valvular cardiomyopathy.
There are no prospective randomized clinical trials for patients with mildly reduced ejection fraction. There is an 8% left ventricular ejection fraction (LVEF) range to define this clinical entity, and the LVEF is subject to variability. Although there are no prospective randomized clinical trials for individuals with heart failure with mildly reduced ejection fraction (HFmrEF), the cut points for ejection fraction have been determined from the clinical trial population to enrich the strategy for the treatment effect and cardiovascular outcomes. However, in 2016, the ESC guidelines identified a gray area in HF, which ranges from 42-49%, called heart failure with mid-range. While the EF is a continuous variable, it is subject to substantial variability, leading to misclassification. The trajectory of LVF over time and the cause are important to evaluate, and one EF measurement at one point in time may not be adequate. The LVEF is not a static measure and changes over time. Therefore, the HFmrEF group is made up of different EF trajectories, which are more important than a static EF measure. Furthermore, this group may not be receiving adequate treatment due to existing clinical inertia and obstacles to implementing guideline-directed medical therapy (GDMT).
American College of Cardiology (ACC) International Congress 2023, 4th March-6th March 2023, New Orleans

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)