ACC 2023: Atrial Fibrillation Ablation: The Sooner the Better? Joint Symposium of the Heart Rhythm Society and the American College of Cardiology
The symposium discusses the timing of ablation for new onset atrial fibrillation (AFib/AF), the use of interrupted or non-interrupted anticoagulation, ablation and survival.
In a study on patients presenting with first episode paroxysmal AFib, almost 50% received no treatment and had no recurrence of an AF episode. Thus, when patients who present with new onset AF do not require to go from the emergency room to an electrophysiology (EP) lab. The ATTEST trial which studied whether catheter ablation or medical therapy to delayed progression of AFib, demonstrated that the rate of persistent AFib was significantly lower with radiofrequency catheter ablation (2.4%) than with antiarrhythmic drug therapy (17.5%) suggesting that ablation in paroxysmal AF can prevent progression to persistent. Large observational registries showed that ablation was associated with lower stroke rates, mortality and slower decline of cognition. The CABANA trial suggested that although ablation was better than drug to prevent AFib, there was no difference between drug and ablation for the primary end points and mortality. The EAST-AFNET 4 trial was stopped for efficacy after 5-years follow-up. The CASTLE AF trial showed poor results with medical therapy as compared to ablation in patients with low ejection fraction.In conclusion, ablation is superior to antiarrhythmic drugs in reducing AFib recurrence and burden. Early ablation in patients with paroxysmal AFib may prevent progression to persistent.
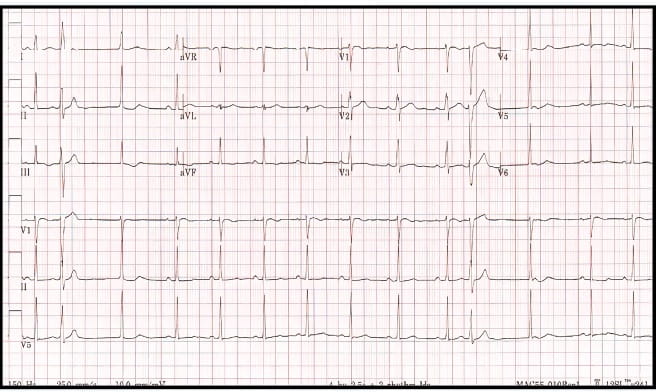
There is a question regarding the choice of using or not using interrupted or non-interrupted anticoagulation for atrial fibrillation ablation. The COMPARE trial demonstrated that there was no significant difference between major bleeding and that the primary endpoint of stroke, transient ischemic attack (TIA) or systemic embolism at 48 hours. A meta-analysis of minimally interrupted or interrupted anticoagulation versus uninterrupted coagulation, showed that thromboembolic events in interrupted were much higher compared to uninterrupted anticoagulation. Studies comparing Rivaroxaban and Apixaban showed no difference in adjudicated events or bleeding events. For Apixaban there was no significant difference in stroke and TIA or bleeding. In general, minimally interrupted direct oral anticoagulants (DOACs) are better than vitamin K agonists; there is no significant difference if the DOAC is interrupted the night before versus uninterrupted the day before. Uninterrupted DOACs should be used in patients who are at a risk of periprocedural stroke. With uninterrupted VKA or minimally interrupted DOACs, there is a decreased use of transesophageal echocardiogram (TEE) Post ablation, long-term coagulation is to be used for at least 2 months; if there is no recurrence of AF or Chad risk score is zero, consider discontinuing anticoagulation. The updated 2019 AHA/ACC/HRS AF guideline recommends 2 months of systemic anticoagulation, at least post ablation, and then consider patients' risk factors for stroke and risk for bleeding.
There is a 5-fold increased risk of developing HF in patients with atrial fibrillation. The CHARM trial has demonstrated that AFib predicts a high risk of cardiovascular morbidity and mortality irrespective of the baseline and patients with AFib and low ejection fraction had an absolute higher risk of adverse cardiovascular outcomes. Ablation produces significant improvement of symptoms in patients with different NYHA classes (Ischemic and non-ischemic). There is also a significant improvement in peak VO2 and ejection fraction. There is almost double a chance of maintaining sinus rhythm with catheter ablation in class 2 or class 3 HF patients. The CASTLE-AF trial demonstrated that in the primary composite endpoint of death and heart failure hospitalization, there was a significant improvement with ablation. Evidence supports catheter ablation to reduce untimely hospitalization, remodelling and with acceptable safety.
AF requires team based care to reduce death, improve outcomes, adhere to guidelines, improve patient satisfaction and quality of life, reduce resource utilization and increase cost-effectiveness. Having a specialized Afib clinic significantly lowers the rate of cardiovascular death and hospitalization from arrhythmia. Nurse-led care in Afib offers improvements in mental health, vitality, physical functioning and reduces symptom frequency and role limitations due to emotional problems. In absence of team-based care, services can be coordinated through a patient navigator, allied healthcare professionals and technology can support several efforts.
American College of Cardiology (ACC) International Congress 2023, 4th March -6th March 2023, New Orleans