"Acute asthma or exacerbations of asthma (asthma attacks) are episodes of progressive increase in shortness of breath, cough, wheezing or chest tightness, or a combination of these symptoms."
Understanding & Managing Acute Asthma
What is Acute Asthma?
Global Initiative for Asthma (GINA) - 2009
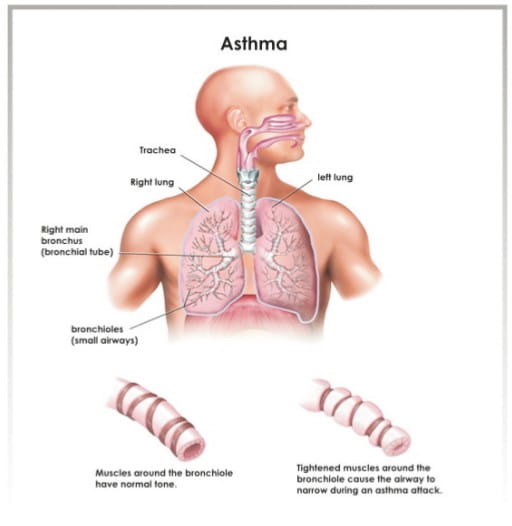
What Happens in Acute Asthma?
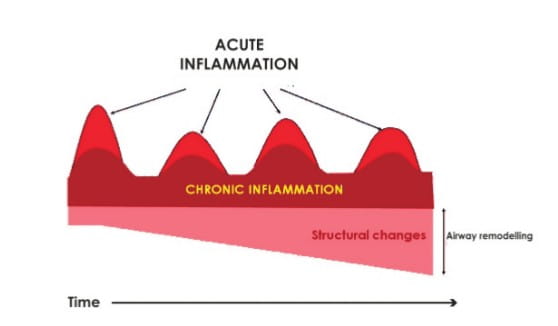
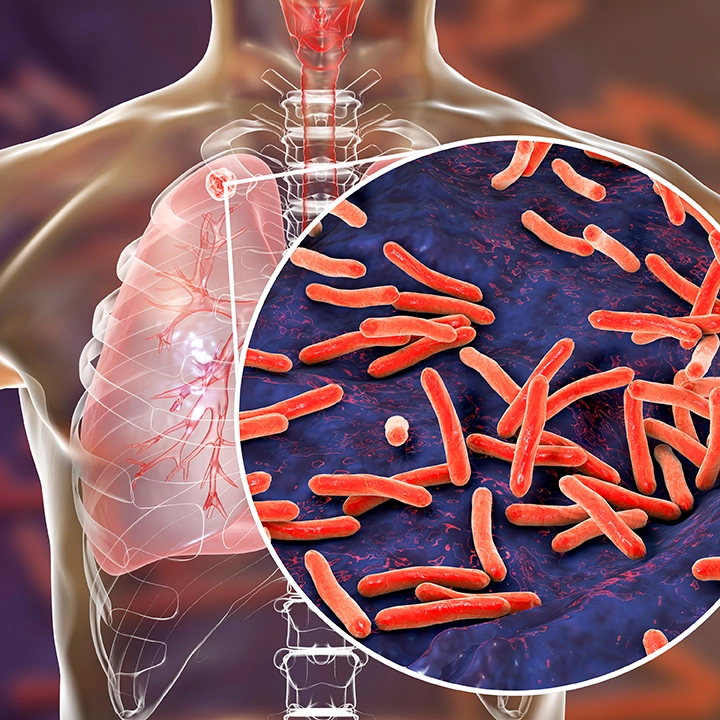
In patients with asthma, the airways are chronically inflamed. This, if untreated, can lead to airway remodelling, i.e. permanent structural changes in the airways.
During acute attacks of asthma along with bronchospasm, there is a flare-up in this inflammation, which has been demonstrated by studies reporting increased levels of inflammatory cells and mediators like eosinophils, interteukin (IL-5, IL-8), eosinophilic cationic protein and leukotrienes.
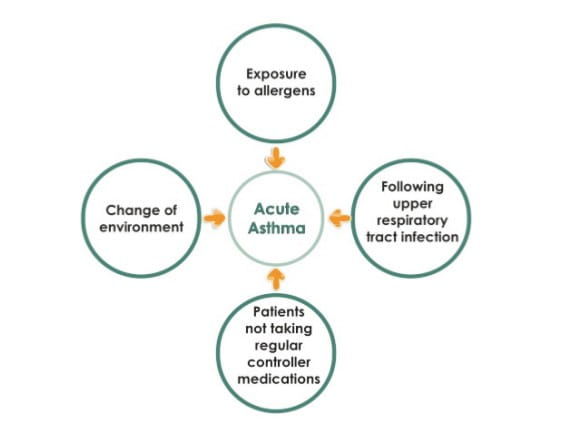
What are the Common Causes of Acute Asthma?
What are the Symptoms of Acute Asthma?
- Breathlessness
- Cough
- Wheezing
- Chest tightness
Which Patients are at High Risk of Acute Asthma?
Patients
- with a history of near-fatal asthma requiring intubation and mechanical ventilation;
- who have had a hospitalization or emergency care visit for asthma in the past year;
- who are currently using or have recently stopped using oral glucocorticosteroids;
- who are not currently using inhaled glucocorticosteroids;
- who are over dependent on a rapid-acting bronchodilator, especially those who use more than one canister of salbutamol (or equivalent) monthly;
- with a history of psychiatric disease or psychosocial problems, including the use of sedatives; and,
- with a history of non-compliance with an asthma medication plan.
These patients require closer attention and should be encouraged to seek urgent care early in the course of their asthma attacks.
All patients with asthma, irrespective of their severity, are at a risk of developing an acute attack.....
How Can You Evaluate Patients with Acute Asthma in the Clinic?
Initial Rapid Assessment
- History, to ascertain the severity of an asthma attack. This includes severity and duration of symptoms, including exercise limitation, sleep disturbance, all current medications (including dosage and device prescribed), dosage usually taken, dosage taken in response to deterioration and patient's response to therapy, time of onset and cause of present asthma attack and risk factors for death from asthma.
- Physical examination, which includes a patient's ability to complete a sentence, auscultation, use of accessory muscles, pulse rate, respiratory rate, peak expiratory flow (PEF) or forced expiratory volume in 1 second (FEV1), oxygen saturation, and arterial blood gas if patient is in extremis
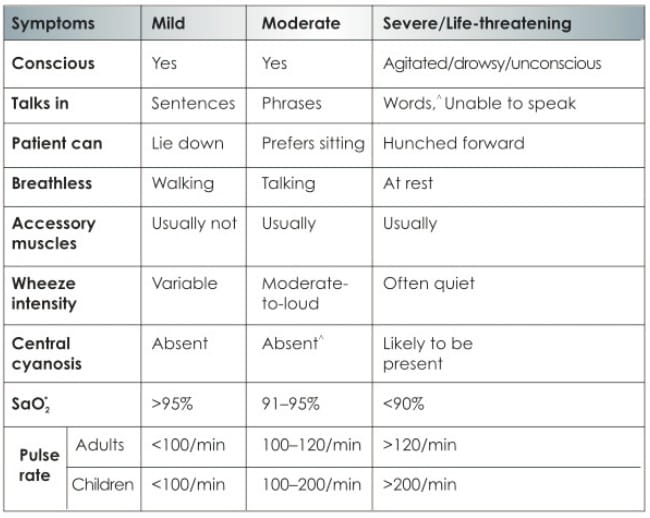
How Can You Judge the Severity of an Acute Asthma attack?
Following are the parameters by which the severity of acute asthma can be evaluated:-
^May be present in adults
*SaO2 - Oxygen saturation in arterial blood
Wheeze is an unreliable indicator of the severity of an asthma attack and may be absent in severe asthma.
-National Asthma Council Australia. 2006
Can Patients Manage Acute Asthma at Home?
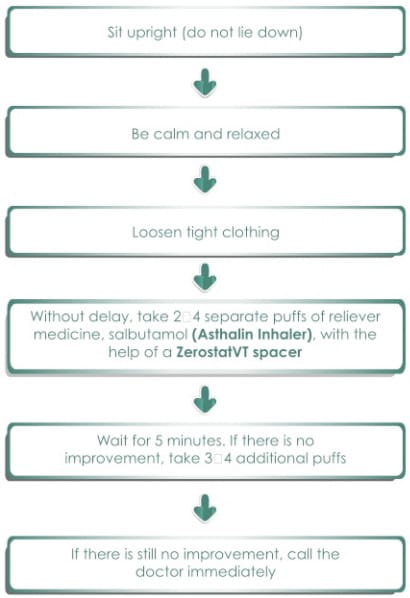
Following are the first-aid tips for patients that would be helpful in case of an acute asthma attack:-
When Should Patients Seek Immediate Medical Care?
- The response to the initial bronchodilator treatment is not prompt and sustained for at least 3 hours.
- There is further deterioration in his/her condition.
- The asthma attack is moderate/severe
- The patient is breathless at rest, is hunched forward, talks in words rather than sentences (if an infant, he or she stops feeding), is agitated, drowsy or confused, has bradycardia, or has a respiratory rate greater than 30 breaths/minute.
- Wheeze is loud or absent.
- Pulse rate is greater than 120/minute (greater than 160/minute for infants).
- Peak expiratory flow rate (PEFR) checked by the peak flow meter (breathe-o meter) is less than 60% of predicted or personal best, even after initial treatment.
- The patient is exhausted.
How Can You Manage Acute Asthma Attacks?
Treatment for Mild-to-Moderate Episodes
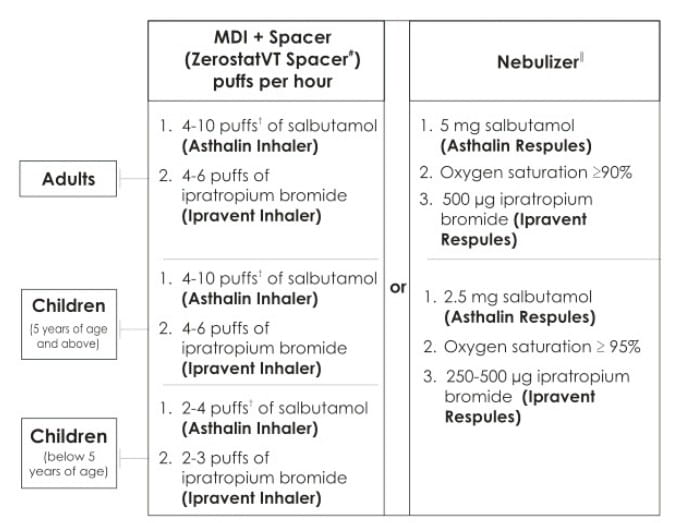
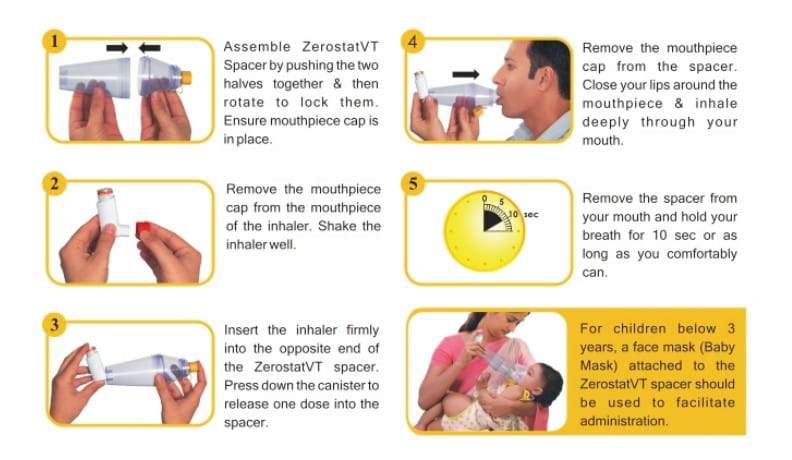
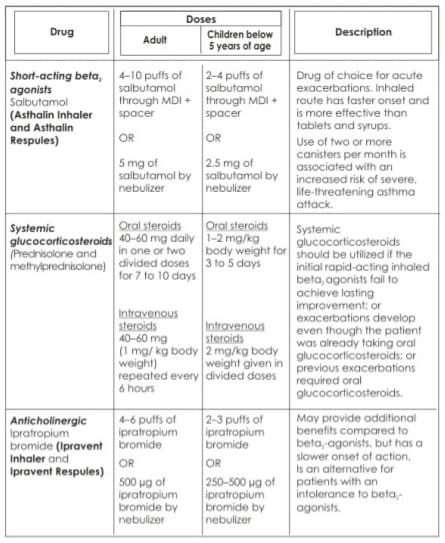
Drugs can be administered either through a metered dose inhaler (MDI) + spacer# or nebulizerI, depending on the severity of acute asthma in a patient.
† Each puff is given separately; the spacer should be loaded with one puff at a time
* To know how to use the ZerostatVT, please refer below
*To know how to use a nebulizer, please refer below
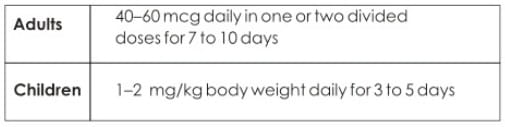
Give oral steroids (Prednisolone Tablets/deflazacort)
Oxygen, at a rate of 6-8 litres/minute, should be delivered through a nebulizer, to maintain SaO2 at 90% or greater for adults and 95% or more in children below 5 years of age. Oxygen saturation should be monitored until a clear response to bronchodilator therapy has occurred.
Inhaled beta2-agonists are the first-line treatment for acute asthma
-British Thoracic Society (BTS) Guidelines. 2008
Subsequent Management
If the Patient's Acute Symptoms Improve
- Continue 2-4 puffs of bronchodilator (Asthalin Inhaler) every 4 hours.
- Hydrate the patient adequately.
- Continue with inhaled steroids if the patient is already on inhaled steroids.
If the Patient's Acute Symptoms Do Not Improve
If the answer to any one of the following questions is positive, then the asthma attack may be severe enough to require hospitalization:
- Is the patient pale or cyanosed?
- Is the patient too wheezy or breathless to talk or eat/feed (in children) or to complete a sentence in one breath (in case of adults)?
- Is the patient using the accessory muscles of respiration?
- Is the pulse rate more than 95?
- Does the patient appear tired and exhausted?
- Is the respiratory rate above 25 breaths/minute for adults and 50 breaths/minute for children?
- Is the heart rate above 110 beats/minute for adults and 140 beats/minute for children?
When Can A Patient Be Discharged From Hospital?
- Patients who demonstrate a rapid response to treatment, observed tor 30 to 60 minutes after the last dose of bronchodilator therapy to ensure stability of response.
- PEF >60% predicted/personal best.
- Sustained on oral/inhaled medication.
- Symptoms are minimal or absent.
Ensure that every patient receives adequate follow-up after an acute asthma episode, including a review of medications, triggers and an asthma action plan.
-National Asthma Council Australia, 2006
How Can Patients Manage Asthma at Home After Discharge?
- Asthalin Inhaler should be used at the time of acute attacks.
- Consider oral steroids (Prednisolone Tablets/deflazacort) and taper down from oral to inhaled steroids.
- Consider a controller inhaler, which is to be used every day to prevent acute conditions.
- Monitor asthma control using a breathe-o meter.
- Patient education and medical follow-up.
The goal of asthma treatment is to achieve and maintain clinical control.
-Global Initiative for Asthma (GINA), 2009
How Can Patients Prevent Future Asthma attacks?
- Inhaled glucocorticosteroids are the most effective controller medications available.
- Inhaled long acting beta2-agonists are most effective when combined with inhaled glucocorticosteroids and this combination is the preferred treatment when a medium dose of inhaled glucocorticosteroid fails to achieve control of asthma.
- Combination therapy prevents asthma exacerbations and also increases patient compliance.
- Inhaled corticosteroids should be used as a maintenance therapy to reduce the frequency of exacerbations in future. Emphasis should be given on the need for regular use of these medications.
- Breathe-o meter should be used daily to monitor and ascertain the severity of asthma.
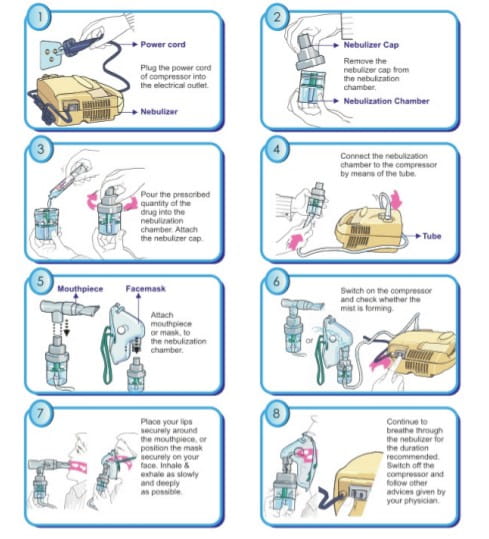
Nebulization therapy for Acute Asthma
Following are the conditions under which nebulization therapy should be chosen:
- Immediate relief is required, which can be achieved only from inhalation therapy.
- Acute asthma/chronic obstructive pulmonary disease (COPD) management requires high doses of drugs (e.g bronchodilators, steroids) along with adequate oxygen supply, which can be conveniently given via a nebulizer.
- Patient is critical/unconscious.
- Where minimal patient cooperation and coordination would be more beneficial, e.g. where patient is unable to coordinate with inhaler devices like pMDI/dry powder inhaler (DPI).
- Patients do not respond to regular treatment.
- Most convenient way to give the optimal dose and for targeted drug delivery.
- Can be used in infants, children and the elderly.
- Home management of severe conditions when a patient is unable to coordinate with other inhalation devices.
- Does not require propellents.
- The aerosol spray that is generated via a nebulizer has a high fine-particle fraction, resulting in highly efficient drug delivery to the lower respiratory tract, so that the nominal dose of drugs delivered by nebulization can be reduced and a very small volume (as little as 0.2 ml) of solution can be aerosolized.
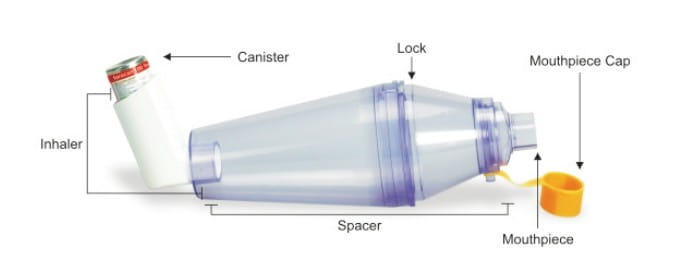
MDI + Spacer therapy for Acute Asthma
- Used in acute symptoms of asthma requiring immediate relief, which can be achieved with inhalation therapy.
- Useful in acute asthma management requiring high doses of bronchodilators and corticosteroids.
- Requires minimal hand-breath coordination.
- Use of the MDI + spacer device is recommended for patients with poor inhalation technique.
- MDI + spacer is an effective alternative and is equally efficacious to a nebulizer in managing acute asthma, especially in children with wheezing.
- Can be used in infants, children and the elderly.
- Inexpensive and easy to use.
- Requires no power source.
- Easily portable.
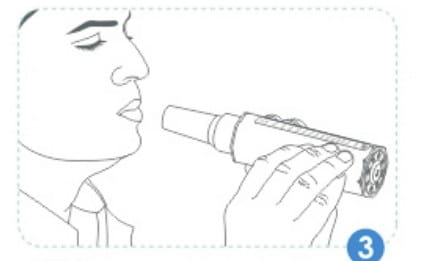
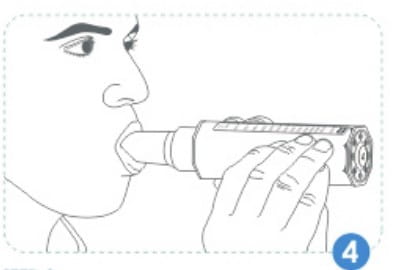
How to Use A Zerostat VT Spacer
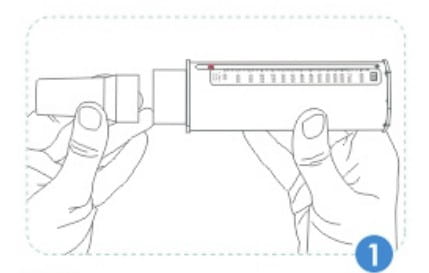
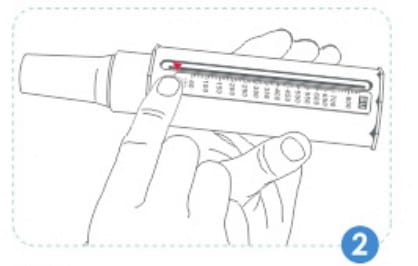
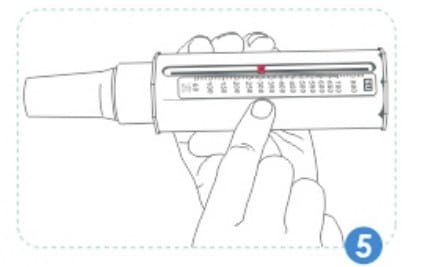
How to Use A Breathe-O Meter
STEP 1
See whether the mouthpiece is fitted into the breathe-o meter. If not, attach it.
STEP 2
Move the pointer along the slot towards the mouthpiece till it does not move any further.
STEP 3
Hold the breathe-o meter so that your fingers are away from the scale & slot. Do not cover the holes at the end of the breathe-o meter.
STEP 4
It is better to take your peak flow reading while standing up. Breathe in deeply. Place the mouthpiece of the breathe-o meter in your mouth. Keep your lips closed firmly around the mouthpiece. Blow out just once as hard and fast as you can. Do not put your tongue inside the mouthpiece, while blowing into the breathe-o meter. If you cough or spit into tho mouthpiece, just take your reading again.
STEP 5
Note where the pointer has stopped on the scale. That number is the peak flow reading.
STEP 6
Repeat steps 2 to 5 twice more, so as to obtain three readings. The highest of the three readings is your peak flow reading. You should take your readings twice a day, first thing in the morning, and then at bed time, or as directed by your doctor.
Monitoring of asthma control, based on the PEF, may have the greatest benefit in patients who cannot readily perceive symptoms of airflow limitation.
-National Asthma Council Australia, 2006
List of Medications Used for Acute Asthma
Oxygen
To achieve arterial oxygen saturation of ≥90% (≥95% in children), oxygen should be administered via nasal cannulae, a mask or, rarely, a head box (in some infants). PaCO2 (partial pressure of carbon dioxide in the arterial blood) may worsen in some patients on 100% oxygen, especially those with more severe airflow obstruction. Oxygen therapy should be titrated against pulse oximetery to maintain satisfactory oxygen saturation.
References
3. National Asthma Council Australia, Asthma Management Handbook, 2006.
4. http://www.aaaai.org/media/statistics/asthma-statistics.asp (Accessed in July 2010).
5. Barnes Peter J. The Changing Face of Asthma. Quarterly Journal of Medicine, New Series 63. No.241, pp. 359-365, May 1987.
6. Oymar Knut and Halvorsen Thomas. Emergency presentation and management of acute severe asthma in children. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2009; 17:40.
7. Agnihotram V. Ramanakumar and Chattopadyay Aparajita. Respiratory Disease Burden in Rural India: A Review from Multiple Data Sources. The Internet Journal of Epidemiology 2005; Volume 2, Number 2.
8. Jeffery Andrew. Acute Asthma: The Foundation Years, 2008; Vol 4. (1):4-8.
9. Papiris Spyros, Kotanidou Anastasia, Malagari Katerina and Roussos Charis. Clinical Review: Severe Asthma. Critical Care 2002; 6:30-44.
10. Skyes Annemarie, Seemungal Terence, ICEAD contributors. Recent advances in exacerbations of asthma. Thorax 2008:63:758-760.
11. Camargo Carlos A, Rachelefsky Gary and Schatz Michael. Managing Asthma Exacerbations in the Emergency Department: Summary of National Asthma Education and Prevention Program Expert Panel Report 3 Guidelines for the Management of Asthma Exacerbations. J Allergy Clin Immunol 2009; 124:S5-14.
12. Jain DG, Singal RK, Jain GB, Clark RA, Chauhan SS. Understanding and Managing Acute Severe and Difficult Asthma. JIACM 2006; 7(4) :316-27.

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)