Doctor's Perception of Diagnosis and Management of Asthma in Malaysia: A Survey of Doctors
Introduction
- For the control of symptoms and prevention of future exacerbations, the Global Initiative for Asthma (GINA) recommendations for the treatment of asthma include use of inhaled corticosteroids (ICS) and ICS combined with long-acting beta2-agonist (LABA) as a controller therapy; short-acting beta2-agonist (SABA) is recommended for reliever therapy (1).
- For diagnosis and monitoring of asthma symptoms, GINA recommends the use of lung function measuring tools such as the spirometer and the peak flow meter. Regular home-monitoring can help to assess the improvement/worsening of symptoms after medication and diurnal variation in the symptoms (1).
- However, in clinical practice, the use of lung function measuring tools to diagnose and monitor asthma is observed to be inadequate. The use of diagnostic tools and treatment strategy is mostly dependent on the doctors’ understanding and perception (2,3,4). Non-pharmacological management of asthma like avoidance of exposure to triggers and smoking cessation is also recommended in the guidelines (1).
- In 1996, the overall prevalence of asthma was reported to be 4.5% and 4.1% in children and adults respectively, in Malaysia (5).
Aim
- This study aimed to evaluate the doctors’ perception about demographics, diagnosis, practice patterns about management and challenges they face in treating their patients with asthma in Malaysia.
Methods
- We conducted a questionnaire-based survey with 17 questions branched out into categories of demographics, prevalence, management and adherence to inhalation therapy.
- Data was collected from spectra of doctors like general physicians, chest physicians and pediatricians practicing in private setting or hospitals, in 14 different locations across Malaysia.
- This study was carried out for a period of 1 month (November 2017) and the total number of doctors targeted was 200.
Results
- A total of 273 doctors responded to the survey totally or partially
- More than 50% doctors see at least 5 patients every day. Approximately 25% of the doctors treated a maximum of pediatric patients (<12 years), whereas, around 45% of the doctors practiced majorly with adults (>25 years) with asthma.
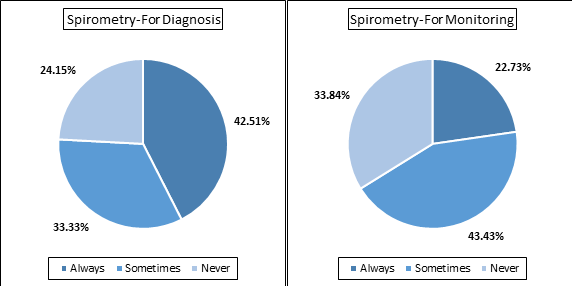
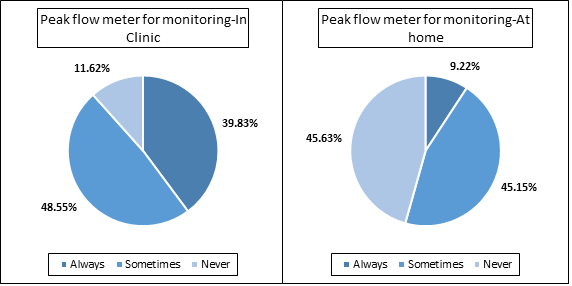
- Only 42.5% of the doctors preferred regular use of spirometry for diagnosis of asthma and approximately 22% of the doctors used it for monitoring the asthma [Figure 2a]. Either always or sometimes, peak flow meter was used by approximately 88% of the doctors for monitoring asthma in the clinic, whereas, around 55% doctors advised using the peak flow meter for home monitoring of asthma [Figure 2b]
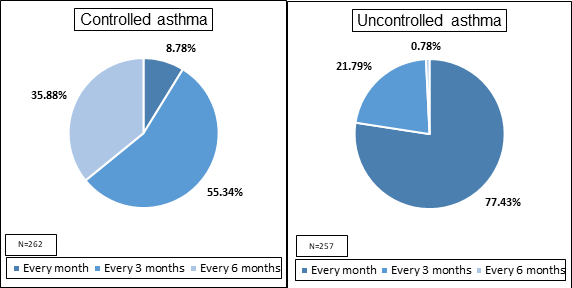
Doctors preferred calling their patients more frequently (every month) for follow-up when their asthma was uncontrolled. For patients with controlled asthma, a period of 3 months and sometimes also 6 months was preferred for follow-up [Figure 3].
|
Q: How often do you suggest a follow-up for your asthma patients, based on control? |
Figure 3: Doctors' approach towards follow-up for asthma patients, based on control
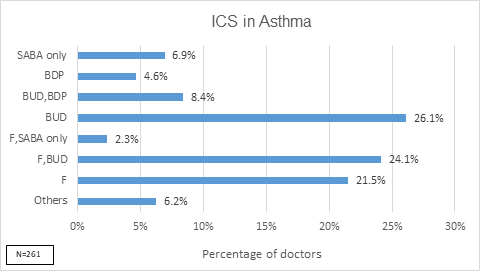
- 26% of the doctors preferred budesonide only, 24% prescribed both fluticasone or budesonide, 21% doctors preferred fluticasone only and 7% doctors prescribed SABA only for management of asthma [Figure 4]
|
Q: If you prescribe an ICS, what is your preferred choice (Select upto two), or do you prescribe a SABA only? |
|
MF=Mometasone furoate; CIC=Ciclesonide; BDP=Beclomethasone dipropionate; BUD=Budesonide; F=Fluticasone; O=Others which include MF + CIC + BDP,CIC + BUD,SABA only + BUD,CIC + F,MF + F,CIC + F,BDP |
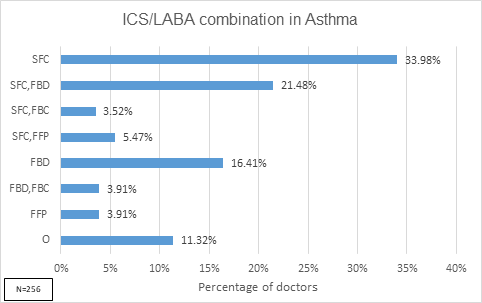
- 34% of the doctors prescribed only salmeterol/fluticasone combination for ICS/LABA, 16% doctors prescribed only formoterol/budesonide combination. 21% doctors preferred either of the two-formoterol/budesonide or salmeterol/fluticasone [Figure 5]
|
Q: Which ICS/LABA combination do you generally prescribe the most? (Select upto two) |
|
SFC=Salmeterol/Fluticasone combination; FBD=Formoterol/Budesonide combination; FBC=Formoterol/Beclomethasone combination; FFP=Formoterol/Fluticasone; VIF=Vilanterol/Fluticasone; *Others which also include SFC,VIF + FBD,FFP + FBD,VIF + FBC + FBC,FFP + FBC,VIF + FBC,O + FFP,VIF + VIF |
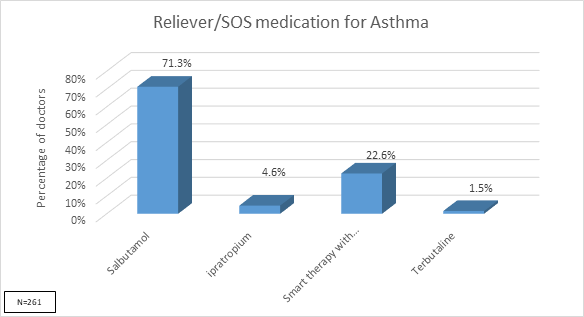
- Salbutamol is prescribed by 71% of the doctors and only 22% doctors prefer SMART therapy with formoterol/budesonide [Figure 6]
|
Q: Which reliever/SOS medications do you prefer to prescribe? |
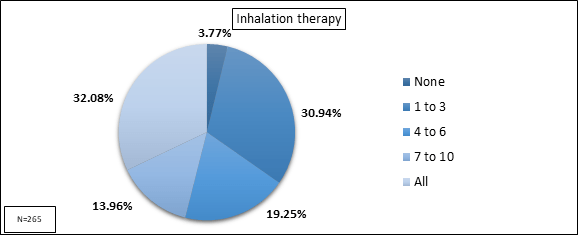
- It was observed that only 32% doctors prescribed inhalation therapy to all their asthma patients [Figure 7]
|
Q: For every 10 patients that visit you, to how many do you prescribe inhalation therapy? |
- Half of the doctors believed that more than 40% of their patients were apprehensive to use inhalers
- Skipping medicine in absence of symptoms was thought to be a major factor for patients’ non-adherence by maximum doctors (71%) followed by incorrect inhaler technique (44% doctors) [Figure 8].
|
Q: In your experience, what do you think are the major factors for patients’ non-adherence to the prescribed treatment? (Can select more than one) |
- 3/4th of the doctors preferred prescribing pMDI-with or without a spacer to most patients with controlled asthma
- Most (95%) doctors believed it would be easier for patients to use a similar device for both reliever and controller.
- Only 44% of the doctors check the inhalation technique of their patients at every visit
- <20% of the doctors said that at least 70% of their patients show good adherence (>80%).
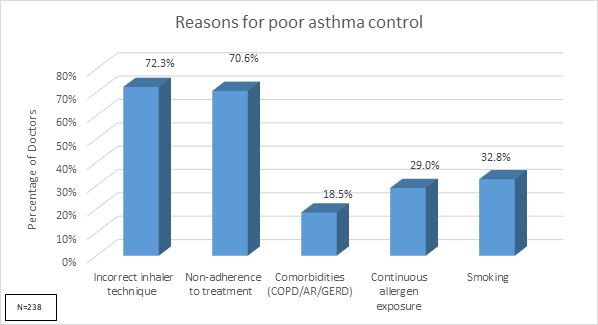
- Around 70% doctors perceived incorrect inhaler technique and non-adherence to treatment as major reasons for poor asthma control [Figure 9].
|
Q: In your experience, what are the major reasons for poor control of asthma symptoms even after being prescribed the adequate treatment? (Can select more than one) |
Conclusions
- In Malaysia, the use of lung function measuring tools such as spirometry could be increased for diagnosis of asthma and use of peak flow meter can be encouraged to use for monitoring symptoms at home.
- Budesonide is the most preferred inhaled corticosteroid; Salmeterol/fluticasone and formoterol/budesonide are the most preferred ICS/LABA combinations. Salbutamol is the most preferred reliever therapy.
- pMDIs are widely prescribed, either with or without a spacer. Almost all doctors believe that a similar device type for both controller and reliever will benefit the patients largely.
- Adherence to inhalation therapy is low and remains a challenge.
References
- Global Initiative for Asthma (GINA). Global strategy for asthma management, updated 2018
- Kotwani A, et al. Indian J Med Res. 2012; 135: 184-92
- Abramson MJ, et al. Prim Care Respir J. 2012; 21(2): 167-73
- Boulet FP, et al. Can Respir J. 2013; 20(4): 256-69
- Ngui R, et al. Med J Malaysia 2011; 66(1): 27-31