The FAST-MI Programme: A Comparison of Five-year Outcomes in STEMI Patients Treated with Early pPCI, Late pPCI or Pharmacoinvasive Strategy
Background
As per the guideline recommendations, acute ST-segment elevation myocardial infarction (STEMI) patients should be treated by default with primary percutaneouscoronary intervention (pPCI) reperfusion strategywhen feasible within 120 min of diagnostic electrocardiogram (ECG). Apharmacoinvasivestrategy(fibrinolysis with referral to PCI centre) is recommended in settings when time from STEMI diagnosis to pPCI exceeds 120mins.With paucity of direct evidence to support the guidelines, in real-world situations, pPCI is often performed beyond the recommended timeline.
Objective
To compare the five-year outcomes in STEMI patients treated with pPCI (timely vs. late) versus those treated with a pharmacoinvasive strategy.
Patient Profile
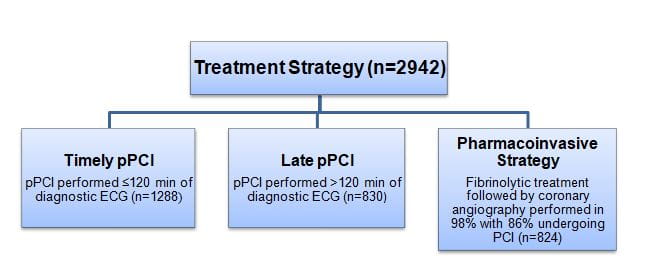
- 2942 patients with STEMI within 12 h of symptom onset and receiving reperfusion therapy with either pPCI or fibrinolytic treatment
Methods
Study Design
- Nationwide multicentre observational study conducted in France, the French registry of Acute ST-elevation and non-ST-elevation Myocardial Infarction (FAST-MI) recruiting patients admitted for AMI every 5 years [2005 and 2010 cohorts]
Treatment Strategy
- The usage of other medicines including; aspirin, beta-blockers, statins, and low molecular weight heparin did not differ significantly in the three study groups. Use of clopidogrel was more frequent in fibrinolytic-treated patients.
Follow-up
- Five years
Endpoints
- Event-free survival at fiveyears
- Combined endpoint of death, acute myocardial infarction (AMI) or stroke at five years
Results
- The five-year survival was higher in the pharmacoinvasive strategy group as compared with thelate pPCIgroup [89.8% vs. 79.5%; adjusted hazard ratio (HR) 1.51; 1.13-2.02], but was similar to that observed in the timelypPCIgroup (88.2%, adjusted HR 1.02; 0.75-1.38).
- As compared to the pharmacoinvasive group, the adjusted HR for the combined endpoint of death, AMI or stroke at five years for timely pPCI group was 1.11 (0.87-1.42, p=0.40) and for late pPCI group was 1.46 (1.14-1.88, p=0.003).
- Nearly 37% of the patients received dominant pharmacoinvasive strategy comprising of full-dose tenecteplase, clopidogrel loading dose ≥300 mgandlow molecular weight heparin. Half-dose fibrinolytic treatment was given to only 2% patients (4% in those aged ≥ 75 years).
- Concordant results were observed in propensity score-matched cohorts and forevent-free survival.
Conclusions
- A substantial proportion of STEMI patients were treated withpPCI beyond recommended timelines.
- Patients treated with pharmacoinvasive treatment at acute stage had improved five-year survival and event-free survival as compared with those treated with late pPCI.
- Event-free survival and five-year survival did not differ significantly in patients treated with early pPCI and pharmacoinvasive treatment.
- Cardiologists should try to ensure that pPCI be performed within 120 min of diagnostic ECG in STEMI patients. In case this timeline cannot be achieved pharmacoinvasive strategy should be instituted to improve long-term and event-free survival, rather than implementing late pPCI strategy
Eur Heart J. Sep 20, 2019 (Published Ahead of Print);doi: 10.1093/eurheartj/ehz665.