Loop Diuretic Dose Change and the Outcomes in Chronic HF Patients: Insights from the ESC-EORP HF Long-Term Registry
22 Dec, 20
Introduction
Amongst patients with chronic heart failure (CHF), it is recommended that loop-diuretics (LD) be down-titrated once euvolemia is achieved. Nevertheless, there is dearth of real-world data on the use of LD in CHF patients. Moreover, the extent of guideline adherence amongst clinicians with respect to this has not been determined.
Aim
- To investigate LD dose changes in daily cardiology practice, agreement with guideline recommendations
- To determine the association between LD dose changes and guideline-directed medical therapy (GDMT) changes
- To determine predictors of successful LD down-titration and the association between dose changes and outcomes
Patient Profile
- Outpatients with HF seen at the participating clinics (n=8130)
- All patients received diuretics prior to and at end of the index visit
- GDMT comprised of beta-blockers, angiotensin converting enzyme inhibitors (ACEi) and/or angiotensin receptor blockers (ARBs) and mineralocorticoid receptor antagonists (MRAs)
Methods
Study Design
- Subgroup analysis of the European Society of Cardiology Heart Failure Long-Term (ESC-EORP) Heart Failure Long-Term Registry
- ESC-EORP Heart Failure Long-Term Registry was a prospective, multinational (conducted across 33 ESC countries), multicentre, observational study of HF patients
Outcomes
- All-cause mortality
- Cardiovascular (CV) mortality
- HF mortality
- HF hospitalization during 1-year following index outpatient visit
- Rates of and predictors of successful LD dose decrease [defined as; decrease of LD during index visit not followed by composite of death, HF hospitalization, New York Heat association (NYHA) class deterioration or subsequent increase in LD dose during 12-month follow-up]
Follow-up
- 12 months
Results
- Mean age of the study population was 66 years and 71% of them were males. Mean ventricular ejection fraction (LVEF) was 37%, 62% HF with reduced EF, 19% HF with mid-range EF, 19% HF with preserved EF.
- Mean LD dose was 61 mg, and median LD dose was 40 mg. Of the entire study population, 40% patients were stable.
- During the index visit 16% patients had their LD dose increased, with the dose increase being more frequent in unstable patients. The LD dose remained stable in 76% patients and was reduced in 8.3% patients. The dose decrease displayed a significant interaction with clinical stability.
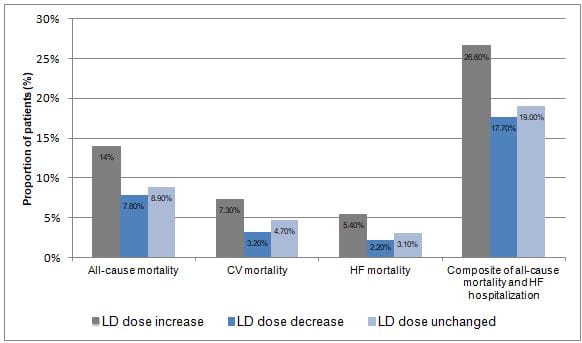
- Increase in LD dose (vs. no change) was significantly associated with HF mortality [hazard ratio (HR) 1.53; P = 0.008] and nominally with CV mortality (HR 1.25; P = 0.103). Fig 1 depicts the outcomes under study as per the LD dose change status.
Fig 1: Outcomes as per the LD dose change status
- Loop diuretic dose increase (vs. decrease) was independently associated with a two-fold increase in the risk of CV mortality (HR 2.01; P = 0.009), a 2.6-fold increase in the risk of HF mortality (HR 2.57; P = 0.003), and nominal increase in the risk of HF hospitalization (HR 1.31; P = 0.063).
- Decrease of LD dose (vs. no change) was associated with nominally lower HF (HR 0.59, 95% CI 0.33–1.07; P = 0.083) and CV mortality (HR 0.62, 95% CI 0.38–1.00; P = 0.052).
- Amongst patients who had their LD dose decreased, higher systolic blood pressure (SBP), and absence of sleep apnea, peripheral congestion, and moderate/severe mitral regurgitation were identified as independent predictors of successful LD dose decrease (Table 1).
Table 1: Predictors of successful LD Dose decrease
|
Predictor |
Odds ratio |
P value |
|
High SBP |
1.11 per 10mmHg increase |
0.032 |
|
Absence of sleep apnea |
0.24 |
0.008 |
|
Absence of peripheral congestion |
0.48 |
0.005 |
|
Absence of moderate/severe mitral regurgitation |
0.57 |
0.008 |
Conclusions
- Amongst a large cohort of chronic HF outpatients, LD dose was unchanged in 76% and decreased in only 8.3% of outpatients. The study depicted high discordance between ‘real-world’ HF patterns and guidelines, with rate of LD dose decrease being disappointingly low.
- As compared to no dose change, increased LD dose was associated with worse outcomes, and decreased LD dose was associated with better outcomes.
- Higher SBP and absence of sleep apnea, peripheral congestion, and moderate/severe mitral regurgitation independently predicted successful LD dose decrease.
- Down-titration of LD dose should be attempted more often in stable euvolemic patients, on the contrary, LD dose should not be reduced and perhaps increased in patients with peripheral congestion.
Eur J HF. 2020; 22:1424-37.

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)