Introduction
A postoperative pulmonary complication (PPC) is the most common serious complication after upper abdominal surgery and are associated with high mortality and costs
Aim
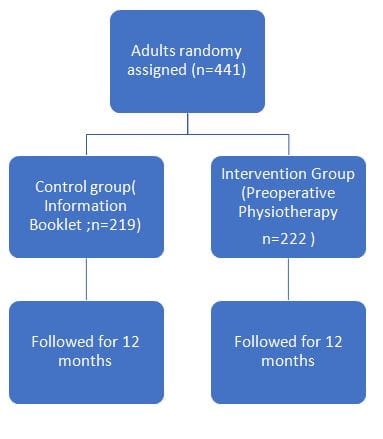
The Lung Infection Prevention Post Surgery Major Abdominal with Pre-Operative Physiotherapy (LIPPSMAck-POP) trial tested the hypothesis that preoperative education and breathing exercise training delivered within six weeks of surgery by physiotherapists reduces the incidence of PPCs after upper abdominal surgery.
Patient Profile
Adults 18 years or older who were awaiting elective upper abdominal surgery that required general anaesthesia, a minimum overnight hospital stay, and a 5 cm or longer incision above, or extending above, the umbilicus, and who attended an outpatient preadmission assessment clinic
Methods
- Prospective, pragmatic, multicentre, patient and assessor-blinded, parallel-group, randomised placebo-controlled superiority trial
Intervention
- Preoperatively, participants received an information booklet (control) or an additional 30-minute physiotherapy education and breathing exercise training session (intervention)
- Education focused on PPCs and their prevention through early ambulation and self-directed breathing exercises to be initiated immediately on regaining consciousness after surgery
- Postoperatively, all participants received standardised early ambulation, and no additional respiratory physiotherapy was provided
Study Outcomes
- The primary outcome was an incidence of a PPC within 14 postoperative days, or hospital discharge, whichever came sooner
- Secondary outcomes included pneumonia,23 defined as the presence of new chest infiltrates on radiography with at least two of the following criteria: temperature >38°C, dyspnoea, cough and purulent sputum, altered respiratory auscultation, and leukocytosis >14 000/mL or leucopenia <3000/mL within the first 14 hospital days, length of hospital stay (acute and subacute inclusive), readiness for hospital discharge24 within the first 21 hospital days, number of days in intensive care or high dependency unit, all-cause unplanned admissions to intensive care or high dependency unit, and hospital costs
Results
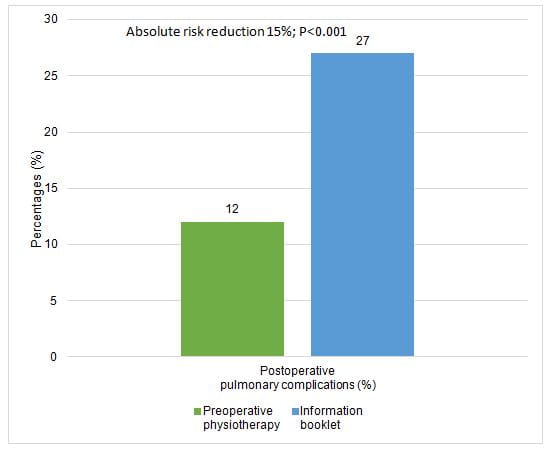
- The incidence of PPCs within 14 postoperative hospital days, including hospital-acquired pneumonia, was halved (adjusted hazard ratio 0.48; P=0.001) in the intervention group compared with the control group, with an absolute risk reduction of 15% and a number needed to treat of 7
- No significant differences in other secondary outcomes were detected
|
Intention to treat |
Preoperative physiotherapy (n=218) |
Information booklet (n=214) |
Adjusted analysis HR, OR, IRR
|
P-value |
|
Pneumonia |
18 (8) |
42 (20) |
0.45 |
0.005 |
|
Hospital utilisation: |
|
|
|
|
|
Median (interquartile range) length of hospital stay (days)* |
8 (6-11) |
9 (7-13) |
0.85 |
0.35 |
|
Sensitivity analysis† |
|
|
1.12 |
0.22 |
|
Ready for hospital discharge (days): |
|
|
|
|
|
Median (interquartile range)* |
6 (5-10) |
7 (5-11) |
0.85 |
0.33 |
|
Sensitivity analysis† |
|
|
1.07 |
0.45 |
|
Median (interquartile range) ICU length of stay (days) |
1.3 (2.9) |
1.5 (2.7) |
0.97 |
0.89 |
|
Unplanned ICU readmissions |
15 (7) |
19 (9) |
0.93 |
0.84 |
|
Hospital readmission at six weeks |
36/197 (18) |
33/199 (17) |
1.14 |
0.59 |
|
Mobility‡ |
|
|
|
|
|
Median (interquartile range) time from operation to ambulation>1 min (hours) |
23 (20-44) |
22 (20-39) |
1.03 |
0.81 |
|
Median (interquartile range) postoperative day achieved >10 mins of ambulation (days) |
3 (1-5) |
3 (1-5) |
0.99 |
0.90 |
|
Median (interquartile range) postoperative day discharged from assisted ambulation (days) |
3 (2-5) |
4 (2-5) |
1.05 |
0.60 |
|
Patient-reported complications at 6 weeks |
|
|
|
|
|
Any complications |
74/192 (39) |
79/197 (40) |
0.90 |
0.50 |
|
Wound infection |
36/192 (19) |
40/197 (20) |
0.88 |
0.50 |
|
Fatigue |
29/192 (14) |
33/197 (14) |
1.00 |
0.99 |
|
Nausea/vomiting/gastrointestinal |
27/192 (14) |
29/197 (14) |
0.98 |
0.94 |
|
Respiratory |
8/192 (4) |
21/197 (9) |
0.45 |
0.059 |
|
Cardiac |
10/192 (5) |
3/197 (2) |
4.06 |
0.036 |
|
Venothromboembolic events |
2/192 (1) |
6/197 (3) |
0.37 |
0.23 |
|
Mean (SD) mortality |
|
|
|
|
|
In hospital |
3 (1.4) |
3 (1.4) |
1.72 |
0.45 |
|
At 6 weeks |
4 (1.8) |
3 (1.4) |
1.47 |
0.62 |
|
At 12 months |
16 (7.3) |
23 (11) |
0.78 |
0.45 |
PPC=postoperative pulmonary complication; ICU=intensive care unit; HR=hazard ratio; OR=odds ratio; IRR=incidence rate ratio.
Analyses are adjusted for baseline age, previous respiratory disease, and hepatobiliary/upper gastrointestinal surgery. Point estimates are HRs for all outcomes except for ORs for prespecified analysis of hospital length of stay and readiness to discharge, unplanned admission to an ICU, length of stay on an ICU, and hospital readmissions at six weeks, and IRRs for patient-reported complications.
*Prespecified analysis involved a rank-ordered comparison of length of stay (days), using mixed-effects ordered logistic regression. OR <1.00 indicates an earlier discharge from hospital.
†Time-to-event analysis with median (interquartile range) number of days reported and estimation of HR using Cox proportion hazards regression. HR >1.00 indicates an increased likelihood of earlier discharge from hospital.
‡No mobility measures are available for patients who did not have upper abdominal surgery.
Conclusion
- Preoperative education and training delivered within six weeks of open upper abdominal surgery by a physiotherapist reduces the incidence of PPCs, including hospital-acquired pneumonia, within the first 14 days after surgery
- This approach could be considered for all patients awaiting upper abdominal surgery
Reference
BMJ 2018;360:j5916