Background
It is uncertain whether an invasive intervention plus medical therapy rather than medical therapy alone results in better clinical outcomes among patients with stable coronary disease (CAD) with moderate or severe ischemia.
Aim
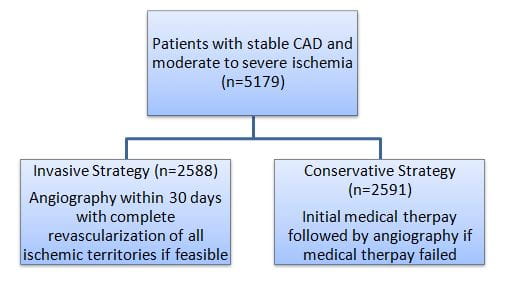
The “International Study of Comparative Health Effectiveness with Medical and Invasive Approaches” (ISCHEMIA) determined the impact of adding cardiac catheterization (angiography) and revascularization when feasible to medical therapy in patients with stable CAD and moderate or severe ischemia.
Patient Profile
- Patients with stable CAD with moderate-severe reversible ischemia (as clinically indicated by a stress test) (n=5179)
Methods
Study Design
- Multinational (conducted across 320 sites in 37 countries) randomized study
Treatment Strategies
- Patients were randomized 1:1 as follows:
- Patents in both the study groups received medical therapy comprising of intensive secondary prevention with lifestyle and pharmacological interventions
Follow-up
- Median follow-up: 3.2 years
- Follow-up visits were conducted at 1.5, 3, 6, and 12 months and every 6 months thereafter
Outcomes
Primary Outcome
- A composite of death from cardiovascular causes, myocardial infarction (MI), or hospitalization for unstable angina, heart failure (HF), or resuscitated cardiac arrest
Secondary Outcome
- A composite of death from cardiovascular causes or MI and angina-related quality of life
Results
- Amongst the invasive strategy patients, 97% underwent angiography and 79% underwent revascularization [percutaneous coronary intervention (PCI); 74%, coronary artery bypass grafting (CABG); 26%).
- Amongst conservative strategy patients, 26% underwent angiography and 21% underwent revascularization. Nineteen percent angiographies and 15% revascularizations were performed before the occurrence of primary outcome event.
- During the follow-up, 318 primary outcome events occurred in the invasive strategy group vs. 352 in the conservative-strategy group. The hazard ratio (HR) with the invasive strategy vs. conservative strategy was 0.93 [95% confidence interval (CI); 0.80-1.08); p=0.34].
- The cumulative event rates did not differ significantly in the conservative strategy group vs. invasive strategy group at 6 months and 5 years (Table 1).
|
|
Invasive Strategy Group |
Conservative Strategy Group |
Difference | |
|
Cumulative event rate |
Cumulative event rate |
Difference |
95% CI | |
|
6 Months |
5.3% |
3.4% |
1.9% |
0.8 to 3.0 |
|
5 years |
16.4% |
18.2% |
−1.8% |
−4.7 to 1.0 |
- With respect to the key secondary outcome, the estimated event rate at 6 months and 5 years did not differ significantly in both the study groups (Table 2).
|
|
Invasive Strategy Group |
Conservative Strategy Group |
Difference | |
|
Cumulative event rate |
Cumulative event rate |
Difference |
95% CI | |
|
6 Months |
4.8% |
2.9% |
1.9% |
0.9 to 3.0 |
|
5 years |
14.2% |
16.5% |
−2.3% |
−5.0 to 0.4 |
- The early increase in the incidence of the primary and key secondary outcomes in the invasive strategy group was attributed to a greater incidence of procedural MI during early follow-up.
- The death rates were comparable in the invasive-strategy group and the conservative-strategy group (145 vs. 144; HR, 1.05; 95% CI, 0.83 to 1.32).
Conclusions
- An initial invasive strategy did not reduce the incidence of primary and key secondary outcomes as compared with an initial conservative strategy in patients with stable CAD and moderate or severe ischemia.
- Patients in the invasive strategy group experienced more procedural MI and lower nonprocedural MI during the follow-up.
- The incidence of death from any cause was low and did not differ significantly among the two study groups
N Engl J Med. 2020 Apr 9;382(15):1395-1407.